Contents
Azospermia: ma'anar, haddasawa, bayyanar cututtuka da jiyya
Yayin duban haihuwa na ma'aurata, ana gudanar da spermogram bisa tsari a cikin namiji. Ta hanyar kimanta ma'auni daban-daban na maniyyi, wannan binciken nazarin halittu yana ba da damar sabunta nau'o'in rashin daidaituwa na maniyyi, kamar azoospermia, rashin cikakkiyar maniyyi.
Menene azoospermia?
Azoospermia cuta ce da ke tattare da rashin cikakkiyar maniyyi a cikin maniyyi. Babu shakka yana haifar da rashin haihuwa ga maza, domin idan babu maniyyi ba za a iya samun hadi ba.
Azospermia yana shafar kasa da 1% na maza a cikin jama'a, ko 5 zuwa 15% na maza marasa haihuwa (1).
Sanadin
Dangane da dalilin, akwai nau'ikan azoospermia guda biyu:
Sirrin azoospermia (ko NOA, don azoospermia mara hana)
Maniyyi yana da rauni ko ba ya nan kuma ƙwayoyin ba sa samar da maniyyi. Dalilin wannan lahani na spermatogenesis na iya zama:
- hormonal, tare da hypogonadism (rashi ko rashin daidaituwa a cikin ɓoyewar hormones na jima'i) wanda zai iya zama na haihuwa (Kallmann-Morsier ciwo alal misali) ko samu, musamman ga ciwon daji na pituitary wanda ke canza aikin hypothalamic-pituitary axis ko bayan magani. (misali chemotherapy);
- kwayoyin halitta: Klinefelter ciwo (kasancewar ƙarin X chromosome), wanda ke shafar 1 a cikin 1200 maza (2), rashin daidaituwa na tsarin chromosomes, (microdeletion, watau asarar guntu, na Y chromosome musamman), canzawa (sashe ɗaya). na chromosome ya rabu kuma yana haɗe zuwa wani). Wadannan abubuwan da ba su da kyau na chromosomal suna da alhakin 5,8% na matsalolin rashin haihuwa na maza (3);
- cryptorchidism na biyu: gwaje-gwajen biyu ba su sauko cikin bursa ba, wanda ke lalata tsarin spermatogenesis;
- kamuwa da cuta: prostatitis, orchitis.
Azoospermia mai toshewa ko mai ban sha'awa (OA, azoospermia mai hanawa)
Gwaje-gwajen suna haifar da spermatozoa amma ba za a iya fitar da su ba saboda toshewar ducts (epididymis, vas deferens ko maniyyi). Dalilin na iya zama na asali:
- nahaihu: an canza sassan seminal daga embryogenesis, wanda ya haifar da rashi na vas deferens. A cikin maza da cystic fibrosis, maye gurbi a cikin kwayar halittar CFTR na iya haifar da rashin vas deferens;
- masu kamuwa da cuta: an toshe hanyoyin iska bayan kamuwa da cuta (epididymitis, prostatovesiculitis, utricle prostate).
Alamun
Babban alamar azoospermia shine rashin haihuwa.
A ganewar asali
Ana yin ganewar asali na azoospermia yayin shawarwarin rashin haihuwa, wanda a cikin maza ya hada da spermogram. Wannan jarrabawa ta ƙunshi nazarin abubuwan da ke cikin maniyyi (maniyyi), tantance ma'auni daban-daban da kwatanta sakamakon da matakan da WHO ta kafa.
A cikin yanayin azoospermia, ba a samun maniyyi bayan an cire dukkanin maniyyi. Don yin ganewar asali, duk da haka, dole ne a yi daya, ko ma wasu nau'i biyu na spermograms, kowane watanni 3, saboda spermatogenesis ( zagayowar samar da maniyyi ) yana kimanin kwanaki 72. Idan babu samar da maniyyi sama da 2 zuwa 3 a jere, za a yi gwajin azoospermia.
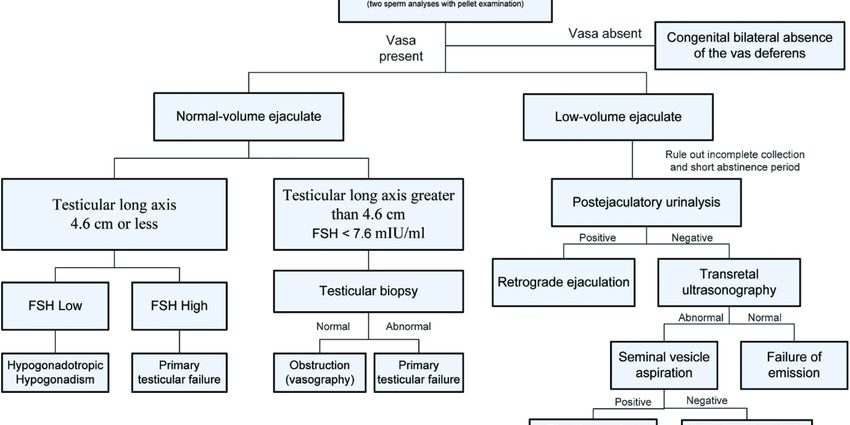
Za a gudanar da ƙarin gwaje-gwaje daban-daban don tace ganewar asali da ƙoƙarin gano dalilin wannan azoospermia:
- jarrabawar asibiti tare da palpation na gwaje-gwaje, ma'auni na ƙarar jini, palpation na epididymis, na vas deferens;
- seminal biochemistry (ko biochemical binciken na maniyyi), domin nazarin daban-daban secretions (zinc, citrate, fructose, carnitine, acid phosphatases, da dai sauransu) kunshe a cikin seminal jini da kuma samo asali daga daban-daban gland shine yake na al'aurar fili (seminal vesicle, prostate). , epididymis). Idan hanyoyin sun toshe, waɗannan sirrukan na iya damuwa kuma binciken biochemical zai iya taimakawa wajen gano matakin cikas;
- Kiwon lafiya na hormonal ta gwajin jini, wanda ya ƙunshi musamman ƙima na FSH (hormone mai ƙarfafa follicle). Babban matakin FSH yana nuna lalacewar ɗigon jini; ƙananan matakin FSH na babban sa hannu (a matakin hypothalamic-pituitary axis);
- serology ta hanyar gwajin jini, don neman kamuwa da cuta, irin su chlamydiae, wanda zai iya haifar da lahani ko lahani ga sashin waje;
- duban dan tayi don duba gwaje-gwajen kuma gano rashin daidaituwa na vas deferens ko epididymis;
- karyotype na jini da gwaje-gwajen kwayoyin halitta don neman rashin daidaituwar kwayoyin halitta;
- biopsy na ƙwanƙwasa wanda ya ƙunshi tattarawa, ƙarƙashin maganin sa barci, wani yanki na nama a cikin ɗigon jini;
- X-ray ko MRI na pituitary gland shine a wasu lokuta ana ba da shi idan ana zargin cutar ta sama.
Jiyya da rigakafi
A cikin abin da ya faru na azoospermia na sirri na asalin hormonal bayan canji na hypothalamic-pituitary axis (hypogonadotropic hypogonadism), ana iya ba da shawarar maganin hormonal don mayar da siginar hormonal da ake bukata don spermatogenesis.
A wasu lokuta, ana iya yin aikin tiyata don neman maniyyi ko dai a cikin gwaje-gwajen a lokacin biopsy na testicular (dabarun da ake kira TESE: TEsticular Sperm Extraction) idan azoospermia ne na sirri, ko kuma a cikin biopsy na testicular. epididymis (dabarun MESA, microsurgical epididymal sperm aspiration) idan azoospermia ne mai toshewa.
Idan an tattara maniyyi, za a iya amfani da su nan da nan bayan biopsy (tarin synchronous) ko kuma bayan daskarewa (tarin asynchronous) yayin IVF (in vitro hadi) tare da ICSI (intracytoplasmic sperm injection). Wannan dabarar AMP ta ƙunshi allurar maniyyi ɗaya kai tsaye a cikin kowane balagagge oocyte. Tunda an zaɓi maniyyi da hadi "tilastawa", ICSI gabaɗaya tana ba da sakamako mafi kyau fiye da IVF na al'ada.
Idan ba a iya tattara maniyyi ba, za a iya ba da IVF tare da gudummawar maniyyi ga ma'aurata.










Ibo ni ile iwosan yin wa