Contents
Achalasia: duk game da esophageal achalasia
Achalasia cuta ce da ke faruwa lokacin da kumburin esophageal ba ya nan ko kuma ba mahaukaci ba, ƙananan kumburin esophageal ba ya annashuwa yadda yakamata, kuma ana ƙara matsin lamba na ƙashin ƙugu na ƙananan esophageal. Makasudin jiyya shine don sauƙaƙa alamun cutar ta hanyar faɗaɗa ƙananan ƙwayar esophageal, ta allurar botulinum toxin, tare da balan -balan, ko ta hanyar yanke tsoffin ƙwayoyin jijiyoyin jiki.
Menene achalasia?
Achalasia, wanda kuma ake kira cardiospasm ko megaesophagus, cuta ce ta motsi na esophagus, wanda ke nuna yanayin rashin jin daɗi lokacin haɗiyewa. Cuta ce da ba a saba gani ba, tana da yawan mutane 9-10 / 100. Yana iya bayyana a kowane zamani, a cikin maza da mata, tare da mafi girman mita tsakanin 000 zuwa 30 shekaru. Yawancin lokaci yana farawa, ta hanyar ɓoye, tsakanin shekarun 40 zuwa 20 kuma sannu a hankali yana haɓaka sama da watanni da yawa ko ma shekaru.
Menene dalilan achalasia?
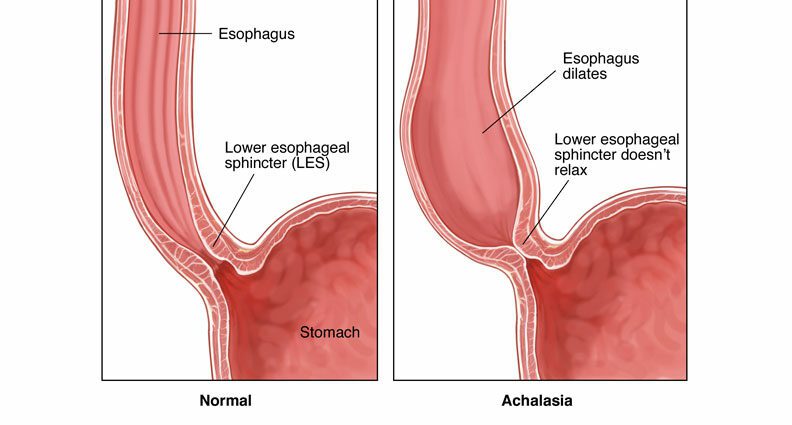
Da zarar an haɗiye shi, abinci yana tafiya cikin ciki ta hanyar murƙushewar tsokar esophageal da ake kira peristalsis. Sannan abinci yana shiga cikin ciki ta hanyar buɗe ƙasan ƙananan esophageal, wanda shine zoben tsoka wanda ke rufe ƙarshen ƙarshen esophagus, don kada abinci da acid na ciki su koma baya. cikin esophagus. Lokacin da kuke hadiyewa, wannan sphincter yana shakatawa koyaushe don ba da damar abinci ya shiga cikin ciki.
A achalasia, munanan abubuwa guda biyu yawanci suna bayyana:
- rashin ƙanƙancewar maƙarƙashiya, ko aperistalsis, wanda ke haifar da lalacewar jijiyoyi a bangon esophagus;
- da rashi ko rashin buɗewa na ƙananan hanjin hanji.
Menene alamun achalasia?
Babban alamar achalasia ita ce cuta. Wannan yana haifar da:
- dysphagia, wato jin toshewar abinci lokacin haɗiyewa ko yayin da yake wucewa ta cikin esophagus, wanda ke cikin kashi 90% na mutanen da ke da achalasia;
- regurgitations, musamman lokacin bacci, na abinci ko abubuwan da ba a narkar da su ba, waɗanda ke tsayawa a cikin mahaifa, suna cikin kashi 70% na lokuta;
- wani lokacin ƙuntata kirji;
- idan marasa lafiya sun sha abinci a cikin huhu, zai iya haifar da tari, kamuwa da cutar numfashi, bronchiectasis watau kumburin bronchi, ko huhun huhu.
Waɗannan alamomin na iya ci gaba na tsawon shekaru da yawa, ba tare da ɓata lokaci ba, kuma suna faruwa tare da abinci mai ƙarfi da / ko ruwa. Suna iya yin sannu a hankali kuma suna haifar da ƙarancin nauyi zuwa matsakaicin nauyi ko ma rashin abinci mai gina jiki. Matsalolin numfashi sun zama ruwan dare, suna shafar 20 zuwa 40% na marasa lafiya.
Yadda za a bi da esophageal achalasia?
Sakamakon ganyen achalasia ya dogara ne akan:
- wani bincike na oesopastro-duodenal endoscopy wanda ke ba da damar lura da rufin esophagus;
- wani x-ray jarrabawa na esophagus, a cikin abin da mara lafiya ingests barite, wani X-ray opaque bambanci matsakaici, wanda ya sa ya yiwu a hango wani dilated esophagus wanda ba ya zubar da kyau;
- kuma a ƙarshe manometry na esophageal, wanda ya sa ya yiwu, godiya ga bincike, don auna matsin lamba tare da esophagus da kuma matakin annashuwa na ƙananan hanji. A yayin da ake yin achalasia, manometry yana lura da rashi na kumburin hanji don mayar da martani ga hadiye ruwa tare da rashin cikakkiyar hutu ko rashin cikakkiyar hutu.
Babu wani magani da zai iya gyara canje -canjen cututtukan cututtukan da ke da alhakin achalasia.
Magungunan da aka ba da shawarar suna da niyyar sauƙaƙe alamun ta hanyar rage matsin lamba na ƙananan hanji da haɓaka haɓakar abin da ke cikin esophageal zuwa ciki ta hanyar tasirin nauyi:
- allurar guba na botulinum a cikin ƙananan hanji na hanji ta hanyar endoscopic yana ba da damar a sake shi. Wannan magani, wanda ake sabuntawa kowane watanni shida zuwa goma sha biyu, galibi ana nuna shi a cikin mafi ƙarancin marasa lafiya a haɗarin tiyata;
- endoscopic dilation, ko bugun huhu, ta amfani da balan -balan da aka sanya a mahaɗin esogastric wanda ya kumbura, kuma wanda ke ba da damar shimfida tsokoki da inganta ɓarkewar esophagus. Yana da tasiri a kusan 80 zuwa 85% na lokuta;
- myotomy tiyata, wanda aka fi sani da Heller, ya ƙunshi yanke tsoffin ƙwayoyin tsoka na ƙananan hanji ta hanyar laparoscopy, dabarar tiyata da ke ba da damar shiga ciki na ciki ta hanyar ƙaramin tiyata. Wannan tsoma bakin, mai tasiri a cikin fiye da 85% na lokuta, gabaɗaya yana da alaƙa da ƙirƙirar bawul a matakin mahaɗin esogastric don iyakance haɗarin reflux gastroesophageal;
- myotomy peroral endoscopic myotomy (POEM) na baya -bayan nan wani yanki ne da aka yi endoscopically. Wannan dabarar, mai tasiri a cikin kashi 90% na lokuta, ya ƙunshi ƙirƙirar rami a bangon esophagus don samun damar kai tsaye zuwa ƙananan hanji don yanke shi.
Wasu jiyya na magunguna na iya taimakawa shakatawa sphincter. Suna da iyakance tasiri amma suna iya tsawaita lokacin tsakanin bugun bulo biyu ko allurar toxin botulinum. Ana iya yin la’akari da su a cikin marasa lafiya waɗanda ke da contraindication ga tiyata ko haɓaka endoscopic, kuma a cikin rashin nasarar magani tare da guba na botulinum. Waɗannan sun haɗa musamman:
- nitrates, kamar isosorbide dinitrate, da za a sanya a ƙarƙashin harshe kafin cin abinci; ana lura da inganta alamun a 53-87% na lokuta;
- Masu toshe tashar sinadarin calcium, kamar nifedipine, suma an sanya su a ƙarƙashin harshe mintuna 30 zuwa 45 kafin cin abinci. An ba da rahoton haɓakawa a cikin dysphagia a cikin 53 zuwa 90% na lokuta.